Abstract
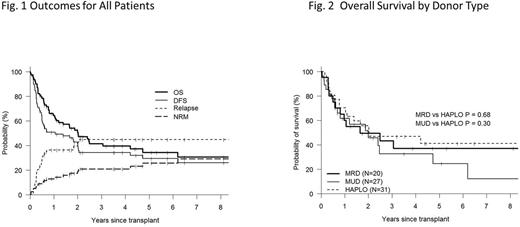
Outcomes following allogeneic hematopoietic cell transplantation (allo-HCT) for AML patients characterized as adverse risk by cytogenetic or molecular criteria have historically been unsatisfactory. Relapse of AML is the primary cause of treatment failure in these patients and can affect the majority of patients with long term survival seen in only a minority of transplanted patients. We evaluated all consecutive patients who underwent first allo-HCT for AML classified as adverse risk on cytogenetic and molecular criteria by the European LeukemiaNet (Dohner et al Blood 2017) at our center between Feb 2003 and Feb 2017 in order to compare outcomes between patients transplanted using a T-replete HLA-haploidentical donor (HID) to those transplanted from a conventional matched sibling (MRD) or optimally matched unrelated donor (MUD). Patient characteristics and outcome data were prospectively entered into our institutional database from which they were retrospectively extracted for this analysis. Our institutional algorithm for donor selection prioritized MRD followed by 8/8 HLA matched MUD. HID were used for patients lacking timely access to a fully matched donor. All patients were treated using standardized supportive care algorithms in the outpatient setting. All HID transplants received GVHD prophylaxis using post-transplant cyclophosphamide (100mg/kg), tacrolimus (d+5 to +180) and MMF (d +5 to +35), MRD and MUD patients received GVHD prophylaxis with tacrolimus and methotrexate. A total of 78 patients were analyzed (HID =31, MUD=27 MRD=20) Patient characteristics were: median age=53 (23-73); male 47%; HCT-CI 0-2=45%, >3=55%; DRI Into=20%, High=65%, v High =15%; ELN adverse risk criterion - complex/monosomal karyotype = 81% , Other adverse cytogenetics = 13% , High-risk mutation =6% ; Disease Status at BMT CR1=60%, other=40%; Graft Source PBSC=85%, BM=15%; Regimen Intensity MAC=63%, RIC/NST =37%. Median follow-up of survivors was 42 months. Patient characteristics were not significantly different between HID, MRD and MUD transplants except that BM was more often the graft source in HID (23%) than MRD (0%) and MUD (15%) (p=0.06). For the entire population and patients with HID, MRD and MUD respectively, 3 year cumulative incidences of non-relapse mortality (NRM) were 21%, 19%, 20% 24% and of relapse were 45%, 42%, 50%, 44%. Three year Kaplan-Meier estimates of overall survival(OS) were 41%, 47%, 43%, 33% and disease-free survival (DFS) were 34%, 39%, 30%, 32% respectively (p=NS for all endpoints on pointwise and global comparisons for donor type). Disease-risk index (DRI) was a significant predictor of three year OS (77% for DRI-intermediate vs 34% for High/v.High, p=0.013 and 0.03 on pointwise and global comparison respectively), DFS (68% vs 26%, p=0.004 and 0.009), relapse (9% vs. 54%, p<0.001 and p=0.002 respectively). Regimen intensity (MAC vs RIC/NST), patient age (<55 vs >55), year of transplant (2003-2011vs 2012-2017) were not significant predictors of any outcome parameter. Female gender was associated with a lower 3 yr NRM (14% vs 29%), and higher OS (52%vs 41%) (p=0.059 and 0.058 on global comparison). These data demonstrate that in patients defined as Adverse Risk by the current ELN classification, three year DFS can be achieved in approximately a third of patients with a NRM of approximately 20%. DRI remains predictive even within this adverse risk cohort. HID donors produce equivalent outcomes to those using optimally matched conventional donors and specifically, relapse rate is not higher following HID even within this high-risk population. Thus, HID may be used to facilitate early transplantation.
Solh: ADC Therapeutics: Research Funding; Celgene: Speakers Bureau; Amgen: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal